One Friday in June 2006, Bob had some blood in his urine – yes like the TV advert. He phoned the GP who said to come in on Monday or go to A&E to get some stronger painkillers over the weekend as it was likely to be kidney stones. A trip to A&E ended up with admission! Shock! Plans for the cricket 20-20 out the window, by Sunday he was on a ward being kept in and they wanted to remove his kidney – wow 48 hours from being “fine” to being “not fine”! Great 52nd birthday present for him – a painkilling jab in the butt! 24 hours later when arriving with our two young sons in tow, I discovered he had been told or rather overheard along with the whole ward that he had cancer. Shell shocked doesn’t really cover it. A few weeks earlier we had walked up Snowdon and now he could hardly walk up the stairs.
Bob had a 2 kilo tumour and kidney removed a few weeks later via keyhole surgery. It took months for him to feel better and after a graduated return to work, Bob was back to work full-time and all seemed well. A few years of scans came and went and life returned to a sort of normal. CT scan then results then waiting for the next CT scan; the cycle continued always on your mind aka Scanxiety!
In 2010 Bob had a persistent sinus problem and was eventually referred to an ENT consultant/surgeon. Within minutes of arriving he was being asked about the cancer and symptoms. When I joked about his snoring, I was curtly told “that was the least of our problems”! A CT scan the following day with results the day after (the NHS can move fast when it needed) showed a mass in his cheek/sinus and would need a biopsy to confirm diagnosis. So yet again a wonderful birthday present for him!
The following week Bob had a biopsy under general anaesthetic and an overnight stay. I arrived at the reception of day surgery and when I said his name the roomful of nurses went quiet, all looked at me then parted to let a woman in scrubs come forward who said “I will take her straight to the theatre…… “.
Bob had decided that attempting to bleed to death on the table was a good idea and lost 2 litres of blood in 20 mins! They had stabilised him but they needed to do an op to cut further risk. So, a short minor op ended up with him being on the table all day (apologies to all those who had their operations cancelled that day). The rest of the day is a bit of a blur but nothing prepares anyone to tell their sons when they come home from school that their Dad is in ICU or one of them asking if their Dad was going to die.
It was a secondary from the kidney cancer and declared inoperable. An x-ray showed blood clots in his lungs, so he was put on blood thinning pills, worrying considering recent events, then a scan showed they were secondary tumours and they took him off the pills. After several weeks his face looked less battered. We were both numb and left in limbo whilst we waited for someone to tell us what would happen next.
Bob’s case was put to the MDT meeting covering all southern hospitals and Guildford agreed they would take him on. It seemed like an eternity between leaving hospital and starting at Guildford and it was good to finally feel like something was going to happen.
The Professor’s team decided one option was a phase II drug trial. We were given a lot of material to digest and returned a week later for Bob sign the consent forms. If he had to be ill, he was going to help doctors and patients in the future. A family member had been part of a trial at the Royal Marsden and another for the measles vaccine back in the 1960s. If we want good medical treatment in this country, we have to help make it better.
The first few days and weeks were taken up with tests, tests and yet more tests. Heart, ECG, bloods, weight, different scans etc. all to provide baseline readings and to make sure all was OK to proceed. It was utterly exhausting emotionally for both of us, as well as physically for Bob. Then the start of treatment… two days of hourly blood tests and ECGs. We had two wonderful trial nurses who had the tortuous job of extracting blood… ironically Bob’s veins hid and refused to give up blood. It became a standing joke over the years at attempts to relieve him of a small phial of red stuff.
4-weekly trips to hospital became the norm with ECGs, blood tests and CT scans at regular intervals and long, long, very long waits for drugs to be dispensed. However it was lovely to walk into a waiting room and for a nurse to stop and say hello and have a chat, talk about our sons and how they were coping, how we were feeling. It made us feel we were not alone. The extra tests a security that all was well. Eventually Bob was well enough to return part time to work. His main side effects from the drugs were fatigue and “digestive issues”.
The drug worked well on the secondaries in his lungs for a year. Then the devastating news, there were changes in his jaw bone metastases. He was removed from the trial.
We saw the maxillo facial surgeons at Guildford who decided that it was better out than in and scheduled surgery for the following month. The drug trial treatment had shrunk the tumour enough for it to be operable. So October 2011 the wonderful surgeons performed a right maxillectomy and fitted him with an obturator (like a big denture).
He was not supposed to be able to talk straight after the op…high as a kite he greeted everyone as he came out of the lift heading towards the ward with a booming hello! Relief! The wounds on his face healed quickly and within a short time even a trainee doctor couldn’t see the lines of the scars.
A scan showed the mets in his lungs had increased so in February 2012 Bob started on Votrient. Within weeks he looked awful. His dose was reduced and the improvement was very quick. Side effects: high BP, indigestion, fatigue and some stomach issues but nothing too major. Thankfully no mouth sores! However, scans showed the pancreas and thyroid had areas of concern but they haven’t changed so just monitored.
After 3 years, increases meant back to the full dose of Paz (this time with only increased fatigue as a side effect) and stability on a CT scan was a great Christmas present.
2016 brought news that the cancer was once again active in his maxilla/sinus area and it was decided to operate again. Bob had surgery and then was moved onto Axitinib. Fatigue hit big time and again a reduced dose worked better. A new treatment, radiotherapy, was tried to attempt to push back the need for further surgery. Two weeks of daily trips were tiring but the team and the doctor meant it was a time with lots of laughter too. November saw our first bit of good news all year: Axitinib was shrinking the other mets by a significant amount.
Sadly a year on, axitinib had failed and a change of drug was needed. We were given two options – cabozantinib and nivolomab. Cabo at the time was only available on an early access scheme which had been fought for by KCSN. Nivolumab, an immunotherapy which had been campaigned for by KCSN. Long discussions with the consultant meant Bob started on cabo as he had responded well to that type of treatment and we didn’t know if NICE was going to allow it in future (they did after much campaigning by KCSN and medical teams).
Initially the dose was too high and Bob was not well. His feet were so bad he could hardly walk, side effects too difficult to cope with and he was taken down to having a lower dose on 5 days a week rather than 7. He began to feel much better. Scans were stable, but in 2018 he started to lose weight, several kilo a month, and scans started to show increases in secondaries. Bob needed a new obturator too, and we spent a lot of time at hospital. I am sure the car went on autopilot.
We were introduced to an oncology dietitian. Bob was put on various supplements and told to eat high calorie food. He was also put onto Creon as he no longer produced enough enzymes to digest his food due to the pancreatic secondaries and the effects of treatment. He was soon putting on weight (as was Maz who has no will power when it comes to nice food!). You have to learn to laugh at “digestive issues” when discussing them with doctors and dietitians to work out how to improve side effects. Laughter is often heard in the dietitian’s room!
Scans were not as good as hoped and in January 2019, the decision was taken to increase the dose to 7 days a week. The side effects increased and the weight loss began again. He was taken off treatment to recover and recently started again on a lower dose and gradually increasing. So far he is feeling much better.
So the next few scans will decide if he changes to a new treatment or carries on. It’s been a tough couple of years, but we still have a laugh. He’s even looking forward to becoming a pensioner this month. Something we didn’t think he would make 13 years ago.
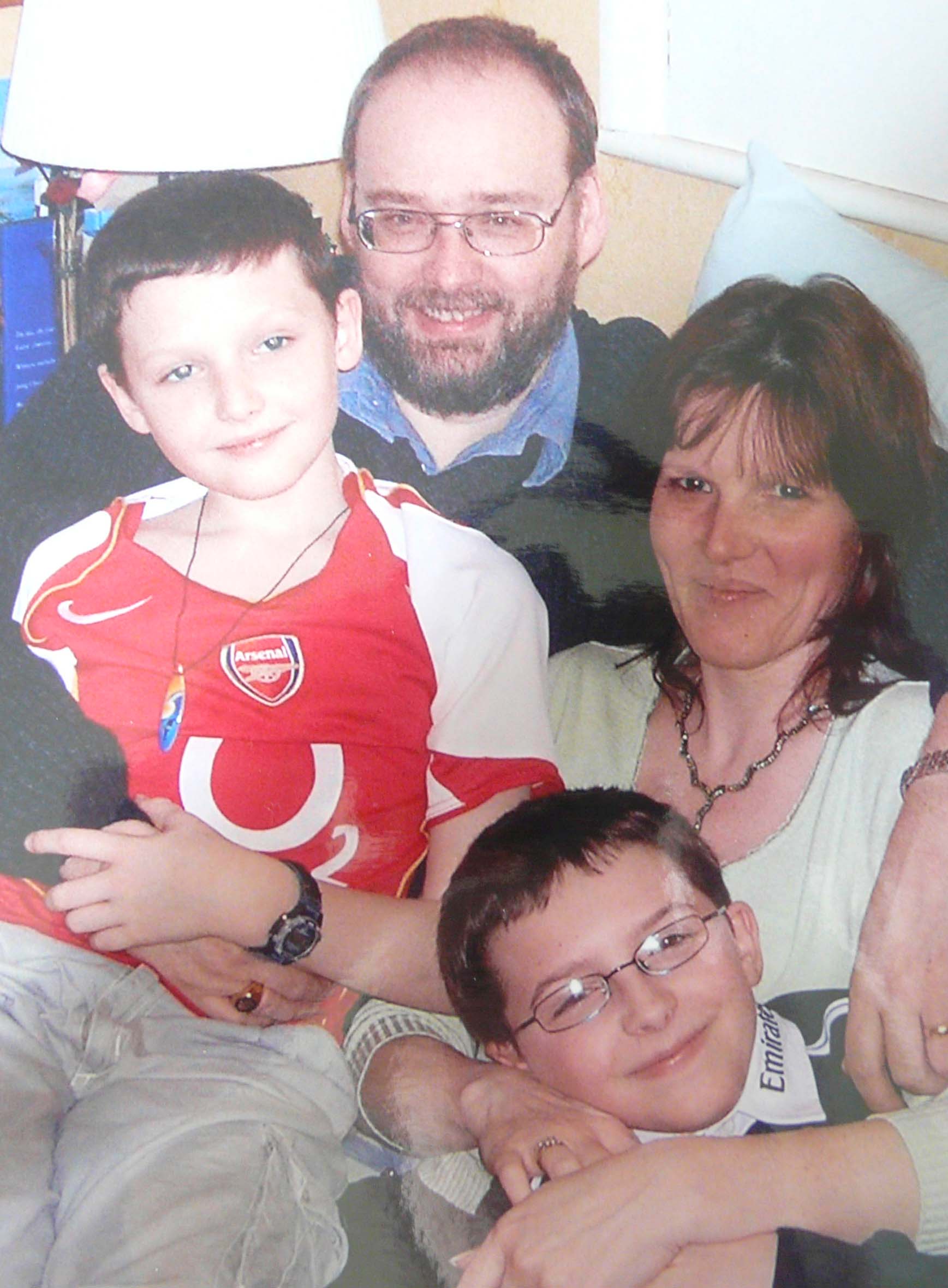
Everyone thinks he looks well and most people have no clue he is ill or has had major surgery on his face. But then they don’t see him the following days when he’s wiped out. The surgeons, doctors and the drug trial have given Bob the chance to see our sons (they were 13 and 11 when Bob was diagnosed) grow up and become amazing young men.
Our advice to anyone with children – be totally honest with them and tell them first. Let them ask questions and don’t make a promise you can’t keep. Gossips at the school gates result in Chinese whispers. It’s true – you do find out who your friends really are! Some have enough of their own problems and can’t deal with someone else’s problems, others just disappeared out of our lives, and some showed true friendship. Our new friends in Kidney Cancer Support Network saved our sanity, understood, gave advice and shared our warped sense of humour and some have become dear friends.
Life, post diagnosis, is different: you learn to grieve for the life you expected to have, come to terms with your new normal and then live that new life. Don’t bottle emotions up and take control of your treatment. Know what should be happening, when and why. Ask questions.
We will be eternally grateful to the patients who put their faith in previous doctors and drug companies and who did the drug trials to enable Bob to be able to have pazopanib, axitinib & cabozantinib.
So nearly 13 years on, we still love the NHS. We owe the consultants, surgeons, radiographers, dietitians and nurses at East Surrey, Redhill and Royal Surrey County Hospital, Guildford everything.
Our lives have been made easier by the lovely receptionists at Guildford and our GP surgery in Old Coulsdon, and we thank them.
[sayit block="1" lang="en-GB" speed="1"]One Friday in June 2006, Bob had some blood in his urine – yes like the TV advert. He phoned the GP who said to come in on Monday or go to A&E to get some stronger painkillers over the weekend as it was likely to be kidney stones. A trip to A&E ended up with admission! Shock! Plans for the cricket 20-20 out the window, by Sunday he was on a ward being kept in and they wanted to remove his kidney – wow 48 hours from being “fine” to being “not fine”! Great 52nd birthday present for him - a painkilling jab in the butt! 24 hours later when arriving with our two young sons in tow, I discovered he had been told or rather overheard along with the whole ward that he had cancer. Shell shocked doesn’t really cover it. A few weeks earlier we had walked up Snowdon and now he could hardly walk up the stairs.
Bob had a 2 kilo tumour and kidney removed a few weeks later via keyhole surgery. It took months for him to feel better and after a graduated return to work, Bob was back to work full-time and all seemed well. A few years of scans came and went and life returned to a sort of normal. CT scan then results then waiting for the next CT scan; the cycle continued always on your mind aka Scanxiety!
In 2010 Bob had a persistent sinus problem and was eventually referred to an ENT consultant/surgeon. Within minutes of arriving he was being asked about the cancer and symptoms. When I joked about his snoring, I was curtly told “that was the least of our problems”! A CT scan the following day with results the day after (the NHS can move fast when it needed) showed a mass in his cheek/sinus and would need a biopsy to confirm diagnosis. So yet again a wonderful birthday present for him!
The following week Bob had a biopsy under general anaesthetic and an overnight stay. I arrived at the reception of day surgery and when I said his name the roomful of nurses went quiet, all looked at me then parted to let a woman in scrubs come forward who said “I will take her straight to the theatre…… “.
Bob had decided that attempting to bleed to death on the table was a good idea and lost 2 litres of blood in 20 mins! They had stabilised him but they needed to do an op to cut further risk. So, a short minor op ended up with him being on the table all day (apologies to all those who had their operations cancelled that day). The rest of the day is a bit of a blur but nothing prepares anyone to tell their sons when they come home from school that their Dad is in ICU or one of them asking if their Dad was going to die.
It was a secondary from the kidney cancer and declared inoperable. An x-ray showed blood clots in his lungs, so he was put on blood thinning pills, worrying considering recent events, then a scan showed they were secondary tumours and they took him off the pills. After several weeks his face looked less battered. We were both numb and left in limbo whilst we waited for someone to tell us what would happen next.
Bob's case was put to the MDT meeting covering all southern hospitals and Guildford agreed they would take him on. It seemed like an eternity between leaving hospital and starting at Guildford and it was good to finally feel like something was going to happen.
The Professor’s team decided one option was a phase II drug trial. We were given a lot of material to digest and returned a week later for Bob sign the consent forms. If he had to be ill, he was going to help doctors and patients in the future. A family member had been part of a trial at the Royal Marsden and another for the measles vaccine back in the 1960s. If we want good medical treatment in this country, we have to help make it better.
The first few days and weeks were taken up with tests, tests and yet more tests. Heart, ECG, bloods, weight, different scans etc. all to provide baseline readings and to make sure all was OK to proceed. It was utterly exhausting emotionally for both of us, as well as physically for Bob. Then the start of treatment… two days of hourly blood tests and ECGs. We had two wonderful trial nurses who had the tortuous job of extracting blood… ironically Bob's veins hid and refused to give up blood. It became a standing joke over the years at attempts to relieve him of a small phial of red stuff.
4-weekly trips to hospital became the norm with ECGs, blood tests and CT scans at regular intervals and long, long, very long waits for drugs to be dispensed. However it was lovely to walk into a waiting room and for a nurse to stop and say hello and have a chat, talk about our sons and how they were coping, how we were feeling. It made us feel we were not alone. The extra tests a security that all was well. Eventually Bob was well enough to return part time to work. His main side effects from the drugs were fatigue and “digestive issues”.
The drug worked well on the secondaries in his lungs for a year. Then the devastating news, there were changes in his jaw bone metastases. He was removed from the trial.
We saw the maxillo facial surgeons at Guildford who decided that it was better out than in and scheduled surgery for the following month. The drug trial treatment had shrunk the tumour enough for it to be operable. So October 2011 the wonderful surgeons performed a right maxillectomy and fitted him with an obturator (like a big denture).
He was not supposed to be able to talk straight after the op…high as a kite he greeted everyone as he came out of the lift heading towards the ward with a booming hello! Relief! The wounds on his face healed quickly and within a short time even a trainee doctor couldn’t see the lines of the scars.
A scan showed the mets in his lungs had increased so in February 2012 Bob started on Votrient. Within weeks he looked awful. His dose was reduced and the improvement was very quick. Side effects: high BP, indigestion, fatigue and some stomach issues but nothing too major. Thankfully no mouth sores! However, scans showed the pancreas and thyroid had areas of concern but they haven’t changed so just monitored.
After 3 years, increases meant back to the full dose of Paz (this time with only increased fatigue as a side effect) and stability on a CT scan was a great Christmas present.
2016 brought news that the cancer was once again active in his maxilla/sinus area and it was decided to operate again. Bob had surgery and then was moved onto Axitinib. Fatigue hit big time and again a reduced dose worked better. A new treatment, radiotherapy, was tried to attempt to push back the need for further surgery. Two weeks of daily trips were tiring but the team and the doctor meant it was a time with lots of laughter too. November saw our first bit of good news all year: Axitinib was shrinking the other mets by a significant amount.
Sadly a year on, axitinib had failed and a change of drug was needed. We were given two options - cabozantinib and nivolomab. Cabo at the time was only available on an early access scheme which had been fought for by KCSN. Nivolumab, an immunotherapy which had been campaigned for by KCSN. Long discussions with the consultant meant Bob started on cabo as he had responded well to that type of treatment and we didn’t know if NICE was going to allow it in future (they did after much campaigning by KCSN and medical teams).
Initially the dose was too high and Bob was not well. His feet were so bad he could hardly walk, side effects too difficult to cope with and he was taken down to having a lower dose on 5 days a week rather than 7. He began to feel much better. Scans were stable, but in 2018 he started to lose weight, several kilo a month, and scans started to show increases in secondaries. Bob needed a new obturator too, and we spent a lot of time at hospital. I am sure the car went on autopilot.
We were introduced to an oncology dietitian. Bob was put on various supplements and told to eat high calorie food. He was also put onto Creon as he no longer produced enough enzymes to digest his food due to the pancreatic secondaries and the effects of treatment. He was soon putting on weight (as was Maz who has no will power when it comes to nice food!). You have to learn to laugh at “digestive issues” when discussing them with doctors and dietitians to work out how to improve side effects. Laughter is often heard in the dietitian's room!
Scans were not as good as hoped and in January 2019, the decision was taken to increase the dose to 7 days a week. The side effects increased and the weight loss began again. He was taken off treatment to recover and recently started again on a lower dose and gradually increasing. So far he is feeling much better.
So the next few scans will decide if he changes to a new treatment or carries on. It's been a tough couple of years, but we still have a laugh. He's even looking forward to becoming a pensioner this month. Something we didn’t think he would make 13 years ago.
Everyone thinks he looks well and most people have no clue he is ill or has had major surgery on his face. But then they don’t see him the following days when he’s wiped out. The surgeons, doctors and the drug trial have given Bob the chance to see our sons (they were 13 and 11 when Bob was diagnosed) grow up and become amazing young men.
Our advice to anyone with children – be totally honest with them and tell them first. Let them ask questions and don’t make a promise you can’t keep. Gossips at the school gates result in Chinese whispers. It’s true – you do find out who your friends really are! Some have enough of their own problems and can’t deal with someone else’s problems, others just disappeared out of our lives, and some showed true friendship. Our new friends in Kidney Cancer Support Network saved our sanity, understood, gave advice and shared our warped sense of humour and some have become dear friends.
Life, post diagnosis, is different: you learn to grieve for the life you expected to have, come to terms with your new normal and then live that new life. Don’t bottle emotions up and take control of your treatment. Know what should be happening, when and why. Ask questions.
We will be eternally grateful to the patients who put their faith in previous doctors and drug companies and who did the drug trials to enable Bob to be able to have pazopanib, axitinib & cabozantinib.
So nearly 13 years on, we still love the NHS. We owe the consultants, surgeons, radiographers, dietitians and nurses at East Surrey, Redhill and Royal Surrey County Hospital, Guildford everything.
Our lives have been made easier by the lovely receptionists at Guildford and our GP surgery in Old Coulsdon, and we thank them.[/sayit]