Share this Page:
At the 2022 European International Kidney Cancer Symposium (EIKCS) in Antwerp, Belgium at the weekend, there was a session about care for the whole patient.
Psychosocial implications of kidney cancer
In a presentation about the psychosocial implications of kidney cancer it was noted that kidney cancer is the 14th most common tumour in the world, and the numbers of people with kidney cancer are increasing This is increasing the burden of kidney cancer on global healthcare systems. In 1990, there were 207,000 new cases; in 2020 there were more than 400,000 new cases. Approximately three quarters of tumours are early stage (stage T1/T2), but there is a large variability in how these tumours appear clinically and treatments are becoming more complex. Also, care and treatment depends on age, other pre-existing diseases, and patient preference.
In summary, there are complex needs for kidney cancer survivors that are primarily psychological and physical. In order to identify these needs, clinicians need to take a holistic, patient-oriented approach to treatment. There is a significant unmet research need, which should incorporate specific stages of disease, treatment, and patient demographics.
Quality of life after renal cell carcinoma treatment
During this presentation the quality of life after renal cell carcinoma (RCC) treatment was discussed. According to the World Health Organization, quality life is “A state of complete physical, mental and social well-being and not merely the absence of disease.” Given that the incidence of RCC is increasing with age, it is important to discuss the quality of life among kidney cancer patients. An ageing population increases the importance of a healthy life, particularly since the estimated cancer-specific survival for localised RCC is 62-86%.
In summary, we need to be able to measure quality of life more accurately, run more randomised clinical studies with long-term follow-up, and quality of life outcomes should be included in all clinical studies. There is significant variety between available studies regarding design, measurement tools, and patient population. Partial nephrectomy seems to be better or similar to radical nephrectomy and has the least negative impact on short-term quality of life.
The role of advocacy in patient care
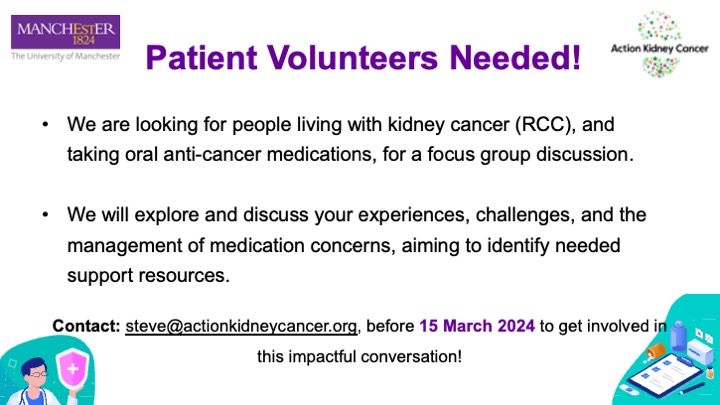
This session addressed non-clinical considerations for caring for the whole kidney cancer patient and discussed the role of advocacy in patient care. The International Kidney Cancer Coalition (IKCC) reaches over 1.2 million kidney cancer patients, with 48 affiliate organisations worldwide. This network addresses unmet needs for kidney cancer patients at the global level.
In 2020, the IKCC Global Patient Survey included over 2,000 patients and carers. The survey included 35 questions on education, experience and awareness, access to care, best practices, quality of life, and unmet psychosocial needs. It covered 41 countries in 13 languages. Overall, 44% of patients were metastatic, 33% had no evidence of disease, and 23% had localised kidney cancer. Key findings included that 42% of patients/carers reported that the likelihood of surviving kidney cancer beyond 5 years was not explained to them. Also, half of the younger patients (<46 years) did not know their tumour subtype. Also, 41% of patients/carers indicated that no one discussed clinical trials with them and 55% indicated that they ‘very often’ or ‘always’ experienced fear of recurrence.
In conclusion, engaging patients leads to better clinical outcomes and patient organisations offer a variety of services and can generate data. Patient representatives are increasingly involved in grant writing/reviewing, clinical trials, manuscripts, ethical committees, resource allocation, health assessment technologies, and clinical guidelines.